A new drug combination may be effective in treating men with metastatic prostate cancer. Preliminary results of this new approach are encouraging and have led to an ongoing international study being conducted in 196 hospitals worldwide.
“We hope to find a well-tolerated and effective treatment to slow the progression of prostate cancer in men with advanced prostate cancer. The approach combines several drugs and attacks the cancer on several fronts,” said Dr. Fred Saad, researcher at the University of Montreal Hospital Research Centre (CRCHUM) and principal investigator of the study.
Antonio Paris, 59, is one of the patients participating in the CRCHUM. “Since I started the new treatment 14 months ago, my cancer first remitted and now is stable,” he said.
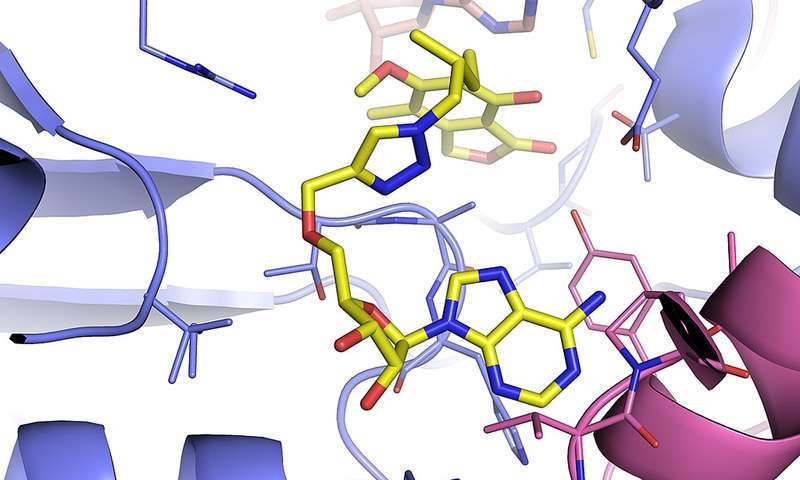
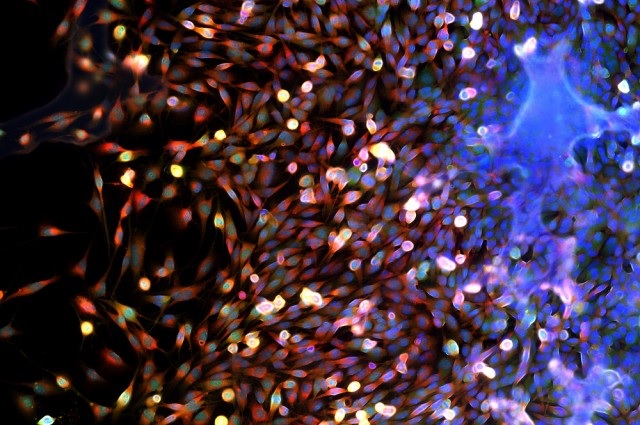
With early detection, prostate cancer is treatable. The vast majority of men recover. But it’s a different story for castration-resistant metastatic prostate cancer. In this most advanced form of the disease, the cancer progresses despite treatment options which include radiation therapy, hormone administration, and even removal of the prostate or testicles. Few options are available to halt the cancer that has spread outside the prostate and is resistant to hormone treatment. Since 2011, abiraterone acetate, sold under the name Zytiga®, has been administered orally in addition to standard hormone treatment. It blocks the production of testosterone, the male hormone, which acts as a fuel for cancerous tumours. “This treatment and other recent advances have extended the survival rates of men with the most advanced stages of prostate cancer while improving their quality of life. Life expectancy has increased from 18 months on average in 2004 to three years in 2015.
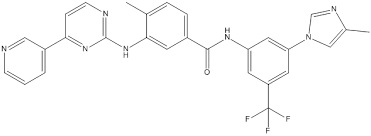
In a Phase 1 clinical trial, researchers tested the safety of a preliminary combination treatment of abiraterone acetate and another drug not yet approved for market, JNJ-56021927. Antonio Paris participated in this initial research phase. “I take 14 pills a day, and it’s going very well. I have the sweats and I’m tired a bit, but it doesn’t stop me from doing all kinds of activities and even renovations,” he said.
“Our trial conducted on forty patients indicate that this treatment is safe. The combined drugs are well tolerated and the treatment appears effective,” said Dr. Saad. Given these encouraging results, the U.S. Food and Drug Administration and Health Canada authorized the start of a Phase 3 clinical study. The trial is designed to compare the efficacy of abiraterone acetate (1000 mg) and a placebo versus treatment combining abiraterone acetate (1000 mg) and JNJ-56021927 (240 mg). In both groups, patients also receive small doses of prednisone to help the treatment and reduce the side effects of abiraterone acetate. Dr. Saad co-directs this randomized, double-blind trial involving 960 patients worldwide.
The findings of this international study will not be known for about another three years. The future treatment will therefore not be marketed for several years. But the researchers are enthusiastic. They hope this first combination treatment will successfully delay progression of the disease and prolong life. And above all, that it will improve the quality of life of patients with this devastating disease.
http://www.eurekalert.org/pub_releases/2015-11/uomh-pdc112415.php